At WiseGEEK, we're committed to delivering accurate, trustworthy information. Our expert-authored content is rigorously fact-checked and sourced from credible authorities. Discover how we uphold the highest standards in providing you with reliable knowledge.
What is Achalasia?
Esophageal achalasia is a rare disorder which prevents the muscles of the esophagus from relaxing properly. People with achalasia have difficulty swallowing because food cannot pass easily from the esophagus into the stomach. The disorder causes a range of digestive symptoms, and can be treated with either medication or surgery.
The main characteristic of this swallowing disorder is that the sphincter muscle of the esophagus is unable to relax. The sphincter is a ring of muscle located at the conjunction of the esophagus and the stomach. When working correctly, the muscle relaxes during swallowing to allow food to pass into the stomach, and remains contracted at other times to prevent the regurgitation of stomach acid and digested food into the esophagus.

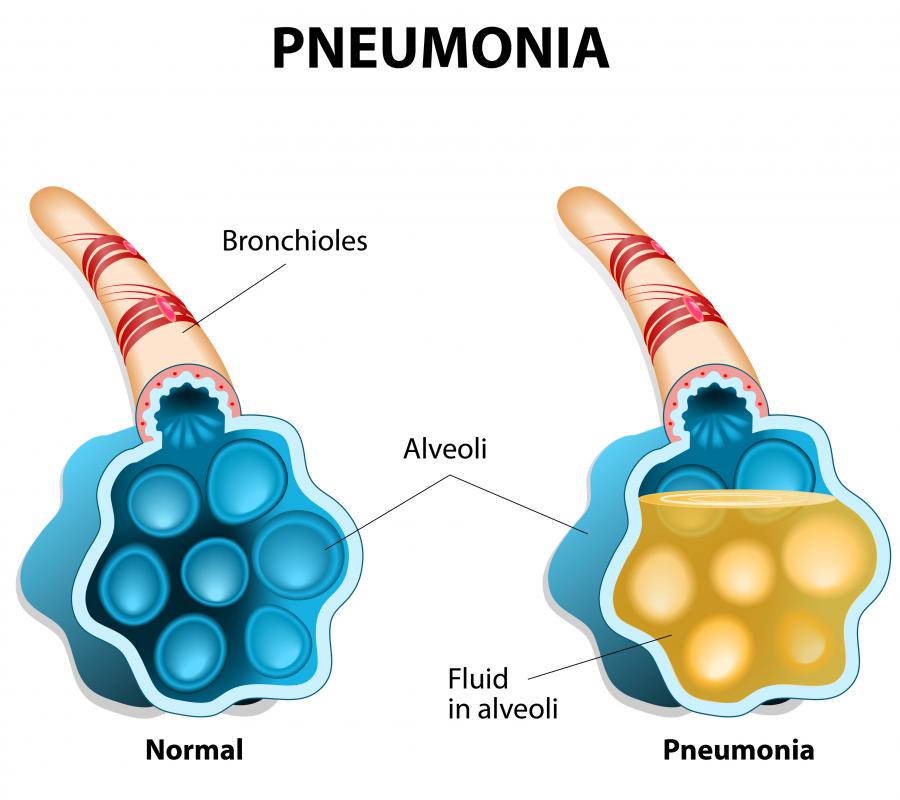
The inability of the sphincter muscle to relax and contract at the appropriate times can cause a variety of gastric effects. Symptoms of this disorder include regurgitation of food or stomach acid, heartburn, cough, and chest pain. Complications such as pneumonia may result if stomach contents are regurgitated into the airways.
Achalasia may be caused by parasitic infection, several types of cancer, or traumatic injury to esophageal nerves. Certain genes may also increase an individual’s susceptibility to developing this disorder. Achalasia treatment focuses on relaxing the esophageal sphincter muscle to make swallowing easier. Treatment options include several types of medication, as well as a surgical procedure. These treatments have similar outcomes, but surgery is a more permanent solution than medication.

The main medication options for this swallowing disorder are calcium channel blockers, and botulinum toxin. Calcium channel blockers are used because they reduce the power of muscle contractions. This reduces the strength of sphincter contraction and makes swallowing easier. Botulinum toxin, also known as Botox®, may be used as a treatment because this toxin, when injected into the sphincter, paralyzes the muscle and prevents strong contractions.

Both of these medications provide only temporary relief from symptoms. Calcium channel blockers may be effective only for a few months, as many people build up tolerance to the drugs. Botulinum toxin has fewer side effects but repeat treatments are needed every six months. In addition the toxin can cause muscle scarring, which may cause complications if surgery is later attempted.

Achalasia surgery is an option for people who do not respond well to medication, or who prefer a permanent treatment over a series of short-term medications. The surgery performed is called a Heller’s myotomy, or esophagomyotomy. In this procedure the sphincter muscle is cut so that the muscle can relax correctly and allow normal swallowing to occur. Patients must be in good physical health to undergo the surgery, as the procedure is a difficult one and recovery can be stressful.
AS FEATURED ON:
AS FEATURED ON:

















Discuss this Article
Post your comments