At WiseGEEK, we're committed to delivering accurate, trustworthy information. Our expert-authored content is rigorously fact-checked and sourced from credible authorities. Discover how we uphold the highest standards in providing you with reliable knowledge.
What is a Stent Thrombosis?
Stent thrombosis is a dangerous condition that occurs when a blood clot forms on a stent. It has symptoms much like cardiac thrombosis of any kind and it is classed by the time in which it occurs after the placement of the stent: very early or first month, early or first year, and late or after a year. A person who has a stent should be aware of sudden feelings of tiredness, inability to draw breath, easy exhaustion, or angina. Additional symptoms might include full myocardial infarction, or heart attack. People could have strong pain in the chest or stomach, difficulty breathing, nausea, pain that shoots down the arm, or any loss of consciousness. This second set of symptoms suggest emergency help is needed, and the first set should be reported to a doctor immediately. Physicians can also help patients by giving them precise instructions on what symptoms need attention.
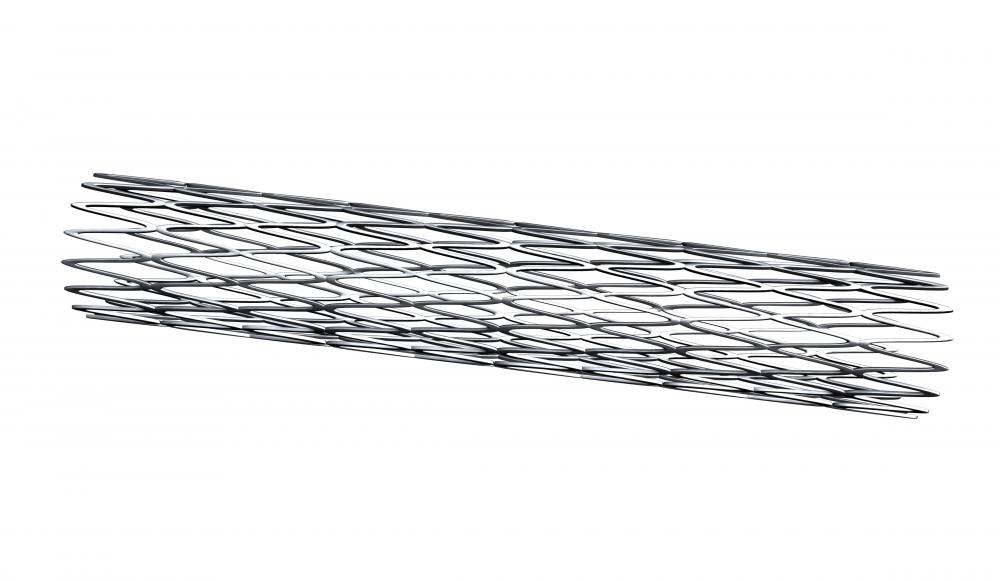
Stents were invented to keep open blood vessels that were narrowed or occluded and they helped to improve heart function for many patients. Risk of restenosis or re-narrowing of the blood vessel led to the development of drug-eluting stents (DES) that released medication. While these effectively decreased risk in one way, they also increased the chances of developing stent thrombosis, especially over a year after the stent placement procedure. This was already a slight risk with simple mesh stents, especially up to a year after placement. When a blood clot forms with either a mesh stent or a DES, a person is at grave risk for death due to cardiac arrest. The medical community continues to study these risks and has specific recommendations on therapy needed after stent placement, and though the prospect of stent thrombosis can be a frightening thing to consider for patients, it should also be recognized as a rare phenomenon.

There are guidelines for prevention of stent thrombosis. When patients receive a stent, they will usually also take two medications that reduce platelet aggregation and production. Since the 2010s medication guidelines have slightly changed. Most people took aspirin and Plavix®, but there is now evidence that some people don’t respond well to the latter. Other drugs besides Plavix® may be recommended instead. Anti-platelet therapy is usually employed for at least a year and longer if a patient has a DES because of heightened risk of late stent thrombosis.

Guidelines also exist for determining which patients make the best candidates for stenting. People with acute coronary syndrome who are having symptoms like chest pain tend to have greater risks for blood clots forming and about 2.5% of this population, according to some studies, will experience blood clots. In contrast, those with stable heart conditions that aren’t presenting that many symptoms have about a 1% risk of problems with blood clot formation. This suggests stent placement is a useful early preventative tool, and may pose more risk for those with more profound disease. Risk is also calculated by the type of stent, and in general a DES has a higher risk than a mesh stent for late stage blood clot formation.
AS FEATURED ON:
AS FEATURED ON:


















Discuss this Article
Post your comments